Fibromyalgia: An effective treatment at our fingertips!
April 24, 2023 - Smart TMS

Effective Fibromyalgia Syndrome (FMS) treatment is in our hands.
Repetitive Transcranial Magnetic Stimulation (rTMS) has been used to treat a range of psychological disorders. And now rTMS is gaining momentum in the treatment of Chronic Pain.
In our previous blog instalment, we highlighted that FMS stems from Central Desensitization – pain originating from the brain. Our knowledge of Chronic Pain and its treatment has progressed a great deal. However many sufferers of FMS struggle to find a treatment that delivers an effective and lasting solution. Chronic pain affects just under 28 million of the UK population. Of that population, 5.4% are FMS sufferers. In your search for Chronic Pain treatment, you will more than likely be presented with three treatment approaches: medication, lifestyle interventions and therapy.
Pills, Pills, Pills.
Research shows that over-the-counter medication will not make a dent in relieving FMS pain. Therefore stronger alternatives are often required. As symptom severity varies across patients, different medications can be utilised to target the ailment that troubles the patient most. Selective Serotonin Reuptake Inhibitors (SSRIs) have often been used in treating depression and have been repurposed for treating FMS too. Studies have shown combinations of SSRIs can reduce morning stiffness, sleep difficulties, and reduce overall pain sensations compared to other treatments (Moret and Briley, 2006).
Therapeutic Intervention Required!
Medication alone to manage FMS is often strongly discouraged. Other therapeutic interventions can be used in combination to manage the day-to-day pain experienced, such as Cognitive Behavioural Therapy (CBT). This can offer FMS patients support by improving their coping strategies, reducing associated depression caused by FMS and improving their overall mood. Moreover, CBT can give you the extra motivation needed to seek out the right treatment needed for a long-term solution (Bernardy, Füber, Köllner and Häuser, 2010).
rTMS: A Solution to Brain Pain
TMS is just one other resource we can add to our “Fibro-Fighting” toolkit. Over a decade of research has been put into its effectiveness for chronic pain disorders. One of the earliest studies by Passard et al found that stimulating an area known as the primary motor cortex. This governs bodily movement and can lead to a decrease in the pain experienced.
In a randomized, double-blind, sham-controlled study, all patients would report their daily average pain in a 24-hour period for one week before starting treatment, to create a baseline. Thereafter, all patients were treated with either rTMS or sham treatment daily for 5 days, before two days without treatment. During treatment, patients then reported their pain daily. When treatment concluded after 15 days, follow-up sessions were arranged at 30 days and 60 days.
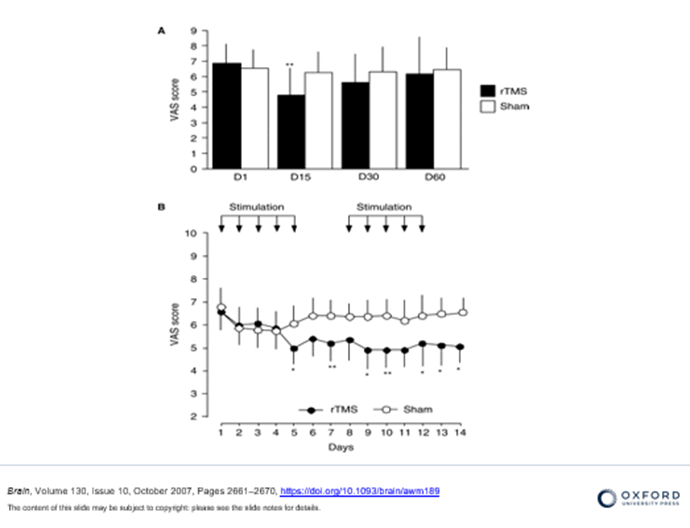
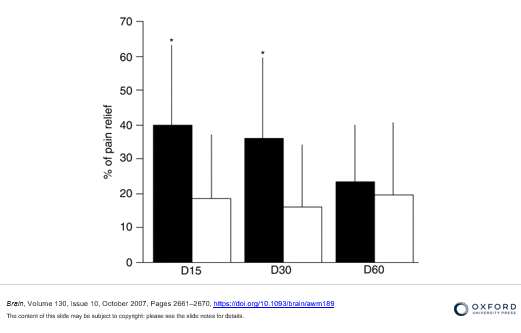
As represented in the graph above, Passard et al demonstrated that rTMS treatment is effective in decreasing pain. This conclusion is based on the Visual Analogue Scale (VAS) that measures subjective pain. It was also found that once rTMS treatment had ceased, there was a gradual increase in pain experienced after 30 and 60 days. Despite this, overall experienced an improvement in their subjective pain experienced. The graph below indicates that overall the percentage of pain relief was greater in the rTMS group (black) compared to the sham group (white).
rTMS has been proven to be effective in treating FMS for extended periods of time. But as we can see from the previous study, the effects can begin to subside, and subjective pain scores begin to creep back up.
Keeping Pain at Bay
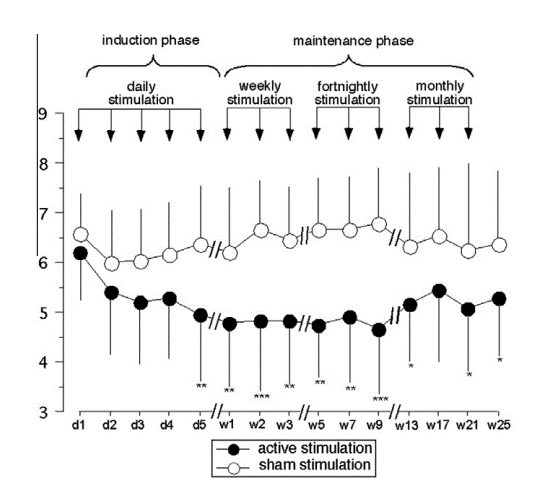
Mhalla et al produced a study that reemphasised how effective rTMS is. Whilst also highlighting the importance of maintenance (or “top-up”) treatments in elongating the effects of rTMS after a successful initial treatment round. After one week of treatment, patients then underwent a ‘‘maintenance phase’’ of 3 sessions one week apart, 3 sessions a fortnight apart, and 3 sessions a month apart. Compared to the sham group, rTMS treatment continued to induce pain relief from day 5 to week 25. Participants experienced an overall long-term improvement. They reported a reduction in overall tiredness and fatigue, a significant reduction in pain in daily activities, such as walking, and improvements in sleep quality.
A Study of Studies
Many other similar studies have been replicated to show rTMS as a treatment option for FMS. However, controversy over its effectiveness still circulated among researchers on its safety and effectiveness. And when there’s uncertainty, that calls for one thing – a meta-analysis! In 2021, Sun et al published a systematic review and meta-analysis of 14 studies, including 433 patients with FMS. They found that rTMS exerted significantly more favourable effects than sham rTMS using the Pain Scale. Once again this concluded rTMS relieved pain and enhanced the quality of life of patients with Fibromyalgia.
Another similar study by Su et al reviewed 18 random control trials containing 643 participants with Fibromyalgia. As expected, they found a significant reduction in their scores on a Fibromyalgia Impact Questionnaire, but they also found improvement in depression and anxiety scores. Fibromyalgia-related depression and anxiety are very common among sufferers, and Su et al conclude that the significant reduction in mental health severity scores is correlated with the analgesic effect of rTMS on FMS.
Conclusion
So concludes our three-part series on Transcranial Magnetic Stimulation treatment and Fibromyalgia. The rising evidence of rTMS treatment gives hope to sufferers who feel as if they have exhausted all their options for relief.
Author, Paul,
Smart TMS Edibnburgh Practitioner
Citations & Image References
Bernardy, K., Füber, N., Köllner, V., & Häuser, W. (2010). Efficacy of cognitive-behavioral therapies in fibromyalgia syndrome—a systematic review and metaanalysis of randomized controlled trials. The journal of Rheumatology, 37(10), 1991-2005.
Mhalla, A., Baudic, S., de Andrade, D. C., Gautron, M., Perrot, S., Teixeira, M. J., … & Bouhassira, D. (2011). Long-term maintenance of the analgesic effects of transcranial magnetic stimulation in fibromyalgia. PAIN®, 152(7), 1478-1485.
Moret, C., & Briley, M. (2006). Antidepressants in the treatment of fibromyalgia. Neuropsychiatric disease and treatment, 2(4), 537-548.
Passard, A., Attal, N., Benadhira, R., Brasseur, L., Saba, G., Sichere, P., … & Bouhassira, D. (2007). Effects of unilateral repetitive transcranial magnetic stimulation of the motor cortex on chronic widespread pain in fibromyalgia. Brain, 130(10), 2661-2670.
Su, Y. C., Guo, Y. H., Hsieh, P. C., & Lin, Y. C. (2021). Efficacy of repetitive transcranial magnetic stimulation in fibromyalgia: a systematic review and meta-analysis of randomized controlled trials. Journal of Clinical Medicine, 10(20), 4669.
Sun, P., Fang, L., Zhang, J., Liu, Y., Wang, G., & Qi, R. (2022). Repetitive transcranial magnetic stimulation for patients with fibromyalgia: a systematic review with meta-analysis. Pain Medicine, 23(3), 499-514.










