Psychiatric Effects of Long Covid
October 2, 2024 - Smart TMS
What is Long Covid?
As we continue to navigate the aftermath of the global COVID-19 pandemic, it is becoming increasingly clear that the virus’s impact extends far beyond the initial infection period. Emerging research reveals a troubling trend: many individuals are experiencing persistent psychiatric and cognitive symptoms long after their recovery from the acute phase of the illness.
This phenomenon, often referred to as “Long COVID,” is raising concerns among medical professionals and researchers alike. In this blog, we delve into the causes of long COVID as well as long-term psychiatric and cognitive effects of COVID-19 as published in a new study conducted by the University of Oxford and University of Leicester.
Risk Factors & Symptoms
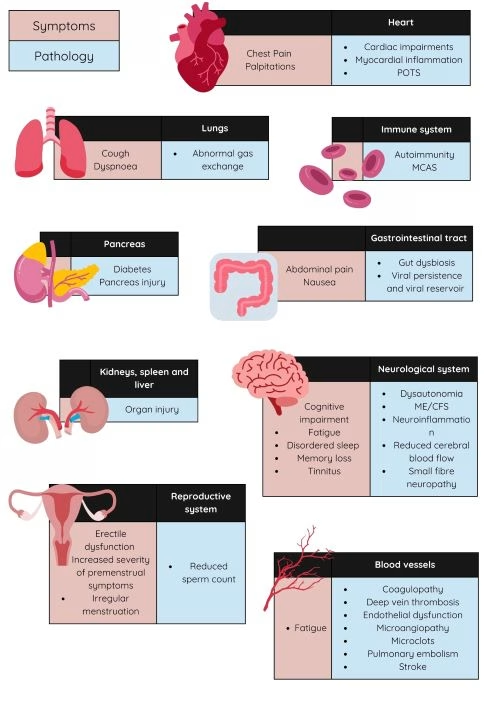
Long COVID is associated with all ages and acute phase disease severities, with the highest percentage of diagnoses between the ages of 36 and 50 years, and most Long COVID cases are in non-hospitalised patients with a mild acute illness, as this population represents the majority of overall COVID-19 cases. Long COVID encompasses multiple adverse outcomes, with common new-onset conditions including cardiovascular, thrombotic and cerebrovascular disease, type 2 diabetes, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia, especially postural orthostatic tachycardia syndrome (POTS).
Risk factors potentially include female sex, type 2 diabetes, EBV reactivation, the presence of specific autoantibodies, connective tissue disorders, attention deficit hyperactivity disorder, chronic urticaria and allergic rhinitis, although a third of people with long COVID have no identified pre-existing conditions6. A higher prevalence of long Covid has been reported in certain ethnicities, including people with Hispanic or Latino heritage.
What are the causes of Long Covid?
There are likely multiple, potentially overlapping, causes of long COVID. Several hypotheses for its pathogenesis have been suggested, including persisting reservoirs of SARS-CoV-2 in tissues; immune dysregulation with or without reactivation of underlying pathogens, including herpesviruses such as Epstein–Barr virus (EBV) and human herpesvirus 6 (HHV-6) among others; impacts of SARS-CoV-2 on the microbiota, including the virome, autoimmunity and priming of the immune system from molecular mimicry; microvascular blood clotting with endothelial dysfunction, and dysfunctional signalling in the brainstem and/or vagus nerve.
Cognitive and psychiatric consequences of Long Covid
As the physical symptoms of long covid take a toll and individual energy levels, sleep, quality of life, these will inevitably also psychologically impact the individual suffering from long covid.
Professor Paul Harrison, Professor of Psychiatry at the University of Oxford said: “Understanding the long-term cognitive and psychiatric consequences of COVID-19 hospitalisation is important for many people, both patients and health professionals alike. We hope these findings will stimulate more research into the development of effective interventions to help prevent and treat these brain consequences of COVID-19.”
A study published in the Lancet Psychiatry reveals the emergence of new symptoms years after COVID-19 was first present, as well as the persistent and significant nature of these symptoms.
The Post-hospitalisation COVID-19 study (PHOSP-COVID) is a prospective, longitudinal cohort study of adults (aged ≥18 years) who were hospitalised with a clinical diagnosis of COVID-19 at participating National Health Service hospitals across the UK.
Key findings of the study
- Cognitive test scores were on average 10 points lower than expected in participants 2-3 years post hospitalisation for COVID. Additionally, a substantial proportion reported severe symptoms of depression (about 1 in 5 people), anxiety (1 in 8), fatigue (1 in 4), and subjective memory problems (1 in 4), with these symptoms worsening over time.
- New symptoms often emerged after 2-3 years in individuals who already exhibited other symptoms at six months post-infection. This suggests that early symptoms can be predictive of later, more severe issues, underscoring the importance of timely management.
- More than one in four participants reported changing their occupation and many gave poor health as a reason. Occupation change was strongly associated with cognitive deficits and not with depression or anxiety.
- The degree of recovery at six months post-COVID-19 is a strong predictor of longer-term psychiatric and cognitive outcomes. Intervening early to manage symptoms could prevent the development of more complex syndromes and improve overall recovery trajectories.
Conclusion
Understanding long COVID is crucial as we continue to uncover the full spectrum of its long-term effects. The research discussed highlights the profound impact that long COVID can have on cognitive and psychiatric health, with symptoms that can persist and even worsen years after the initial infection. This emerging knowledge underscores the importance of early intervention and tailored treatments to help those affected navigate the challenges posed by long COVID. As awareness grows, so too must our commitment to supporting patients, advancing research, and developing effective strategies to mitigate the long-term consequences of this complex condition.
Written by Smart TMS Southampton Practitioner, Roxana










